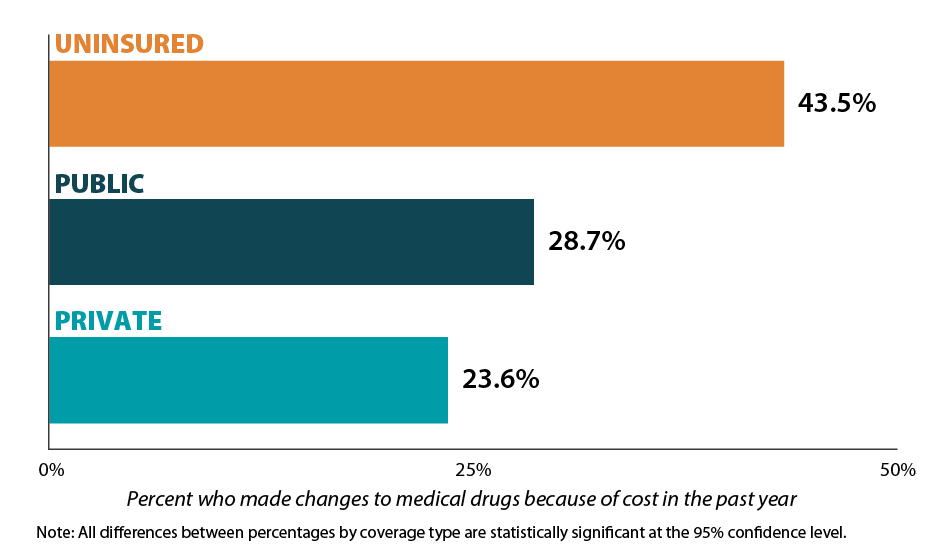
Percent who made changes to medical drugs because of cost in the past year
Measure Overview
The cost of medical drugs in the United States is significantly higher than in other nations. Rising medical drug prices in recent years have made it difficult for some Americans to afford their prescriptions. As a result, individuals may alter their medical drug consumption behavior out of financial necessity, such as asking their doctor for cheaper medications, delaying refills, taking less medication than prescribed, skipping dosages, using alternative therapies, or buying medications out of the country. Measuring changes in medical drug consumption behavior is an important consideration when assessing health care affordability in the U.S.
State Health Compare provides annual, state-level rates of individuals who made changes to their medical drugs in the past 12 months due to cost. These rates are available across three different breakdowns: year, type of health insurance (private, public, or uninsured), and age group (either 19-64 years or 65 and older).
Generate customized graphics using this data by selecting one of the options below.
Related Product
A State-level Measure of Drug Affordability on State Health Compare: Made Changes to Medical Drugs Because of Cost
In 2016 Americans spent more on prescription medications per capita than residents of any other nation due to higher U.S. drug prices. This blog uses 2016 National Health Interview Survey data & estimates to analyze state variation in cost-related drug changes by age group, coverage type. State Health Compare is the only source of state-level estimates for this measure.
A Post-Pandemic Look at the Cost of Employer-Sponsored Insurance (ESI) Coverage: Data from the 2023 Medical Expenditure Panel Survey (MEPS)
In this brief, SHADAC researchers use data from the Medical Expenditure Panel Survey (MEPS) to analyze the private-sector ESI (employer-sponsored insurance) landscape both on the state-level and nationally. Specifically, this brief looks at the post-pandemic landscape of ESI insurance costs and coverage.
